From Latin America to Africa and from Asia to Europe, the pandemic has cost millions of lives. At the same time, it has affected people’s ability to access essential health services. In many places, the devastating knock-on effects of the pandemic have left people without life-saving assistance. MSF teams working in more than 70 countries around the world have often struggled to respond both to the direct consequences of COVID-19 and to other medical emergencies, while dealing with restrictions on travel and impacts on essential medical supplies.

THE KNOCK-ON EFFECTS OF COVID-19
Venezuela
A STRUGGLING HEALTH SYSTEM
In a country where the health system has all but collapsed, COVID-19 has prevented even more people from accessing medical care, whether for chronic diseases or for emergency care for their children.
THE KNOCK-ON EFFECTS OF COVID-19
France
THE VIRUS HITS EUROPE
Europe has not escaped COVID-19 nor the constraints it has brought – indeed at times it has been the epicentre of the pandemic.


THE KNOCK-ON EFFECTS OF COVID-19
Central African Republic
LOW DEATHS BUT HIGH IMPACT
Central African Republic (CAR) is one of many African nations where the pandemic did not reach the catastrophic levels predicted. While this is a huge relief, the knock-on effects of COVID-19 on the fragile healthcare system have been considerable.
Venezuela

In a country where the health system has all but collapsed, COVID-19 has prevented even more people from accessing medical care, whether for chronic diseases or for emergency care for their children. In the capital, Caracas, MSF’s project for survivors of sexual violence had to scale back its services after half of its staff were redeployed to the COVID-19 response. Many of MSF’s patients have been unable to reach the hospital due to travel restrictions. But despite the obstacles, the reduced team has worked around the clock to support patients in every way they can. Dulce, Yamilette and Alberto are three people with a shared message that has sadly become all too familiar in Venezuela.
Alberto is a motorbike taxi driver. His four-year-old son has respiratory problems. The only way he can get treatment for his son is to wait until an appointment becomes available.
Yamilette is a single mother with four children. For months she has had pains in her hips that have prevented her from going out to work. Despite her urgent medical needs, she was turned away from a number of hospitals, all of which were prioritising COVID-19 patients.
People wait in a queue to see a doctor
When COVID-19 hit Venezuela, the country was already immersed in a long-lasting economic and humanitarian crisis, which has been exacerbated by the pandemic. With a collapsing health service struggling to response to people’s basic medical needs, the indirect effects of the pandemic have seen many Venezuelans unable to get medical care.
Dulce is a medical specialist at MSF’s project for survivors of sexual violence in Vargas hospital in Venezuela’s capital, Caracas. Her daily workload changed dramatically when COVID-19 hit the country and MSF was forced to rethink how it could continue to support patients. When the pandemic finally ends, Dulce knows what she will do first.
France

Europe has not escaped COVID-19 nor the constraints it has brought – indeed at times it has been the epicentre of the pandemic. From France and Belgium to Spain and Italy, there have been periods when hospitals have reached maximum capacity and healthcare staff have had to work 24-hour shifts. All of this has impacted care for patients with medical conditions not related to COVID-19. In Paris, many homeless people, including migrants and asylum seekers, have had to cope with changes to, or even the closure of, their usual care facilities or the associations that support them. In response, MSF teams have been running mobile clinics for people living on the streets, many of whom are the invisible victims of the knock-on effects of COVID-19.
Seco is from Gambia and lives on the streets of Paris. Like many other homeless people, he has had difficulties getting medical treatment for his skin condition during the pandemic. With no information on where to go for medical care, his only option is MSF’s mobile clinic, which provides COVID-19 tests and general healthcare to people living on the streets
Mobile clinics for homeless people
Jean-François Véran is project coordinator of MSF’s mobile clinics in France. He has seen a change in the types of people coming for food distributions and basic medical assistance in Paris during the COVID-19 pandemic. But despite everything he has witnessed, Jean-François is optimistic and is looking forward to a future where physical distancing and COVID-19 tests are no longer a daily reality.
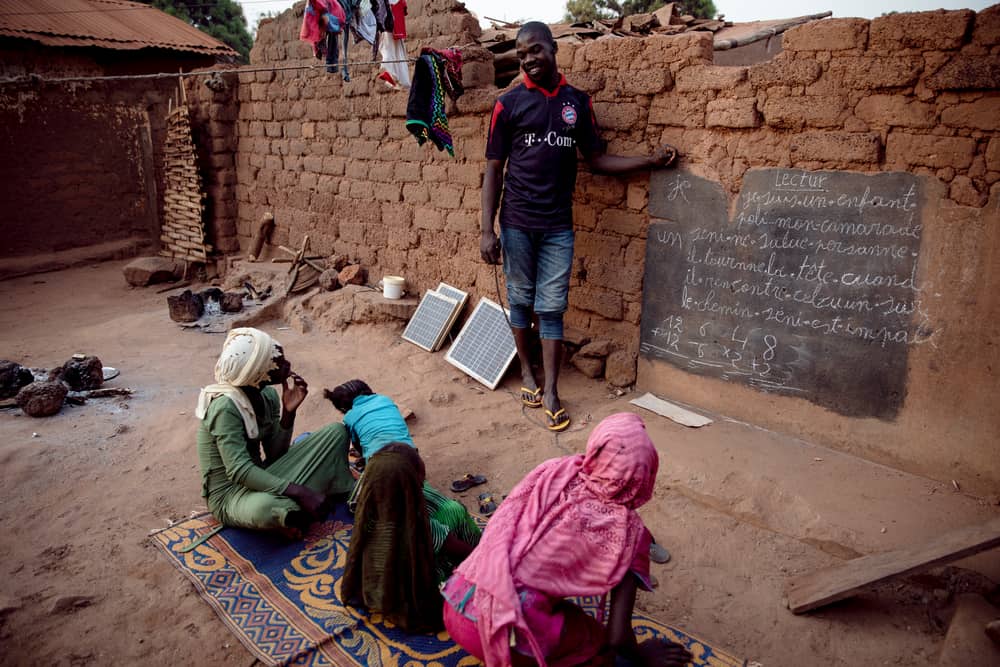
Central African Republic

Central African Republic (CAR) is one of many African nations where the pandemic did not reach the catastrophic levels predicted. While this is a huge relief, the knock-on effects of COVID-19 on the fragile healthcare system have been considerable. Vaccination and treatment for diseases such as malaria, malnutrition and measles are just a few examples of lifesaving activities that have been forced to reduce. Although the pandemic has not hit as predicted, MSF staff continue to follow the situation closely. Any outbreak could be devastating, especially now that the country is engulfed in renewed violence.
Zara works in MSF’s COVID-19 triage unit in Bambari, Central African Republic. Her main concern is how the country’s weak health system and struggling hospitals will manage to respond to COVID-19 at the same time as dealing with so many other medical needs.
Mobile clinics for homeless people
Despite his best efforts, Fidèle, in charge of paediatric triage in Bambari hospital, says it is very difficult to protect his patients from COVID-19 when people have so many other urgent medical needs.
-
Related:
- coronavirus
- COVID-19
- Pandemic