When an MSF team working in the Kenyan city of Mombasa discovered that there were significant gaps in healthcare for adolescents and young people, they decided to do something about it. The assessment they conducted in May 2021 revealed that, among them, the people who found it hardest to get healthcare were often those with specific or unique health needs.
“Key populations”, as they are usually called, have been defined by the Ministry of Health as those who may have unique health needs, including sex workers, people who use drugs, transgender and gender non-binary people, and sexual minority groups (e.g., men who have sex with men, women who have sex with women) and other special vulnerable groups such as street populations. These groups often experience a greater prevalence of health risks and mental health issues, while also enduring a higher degree of marginalization compared to their counterparts.

he MSF team discovered that the most glaring gaps were in sexual and reproductive healthcare. Many of the young people they spoke to had experienced teenage pregnancies, unsafe abortions and sexual and gender-based violence, yet had not received appropriate counselling or treatment. Additionally, some had unmet psychosocial needs but had not been provided with mental healthcare services.
“It is vital that these groups of people can access health facilities for consultations and regular check-ups without fear,” says Tamariz.
“When you show them that you care, they open up”
Working closely with the Mombasa County Department of Health, MSF launched its Adolescent and Youth-Friendly Services in 2021. The aim was to make it easier for young people aged 10 to 24 who found themselves marginalised or excluded from healthcare, for whatever reason, to get the advice and treatment they need.

Youth-friendly spaces
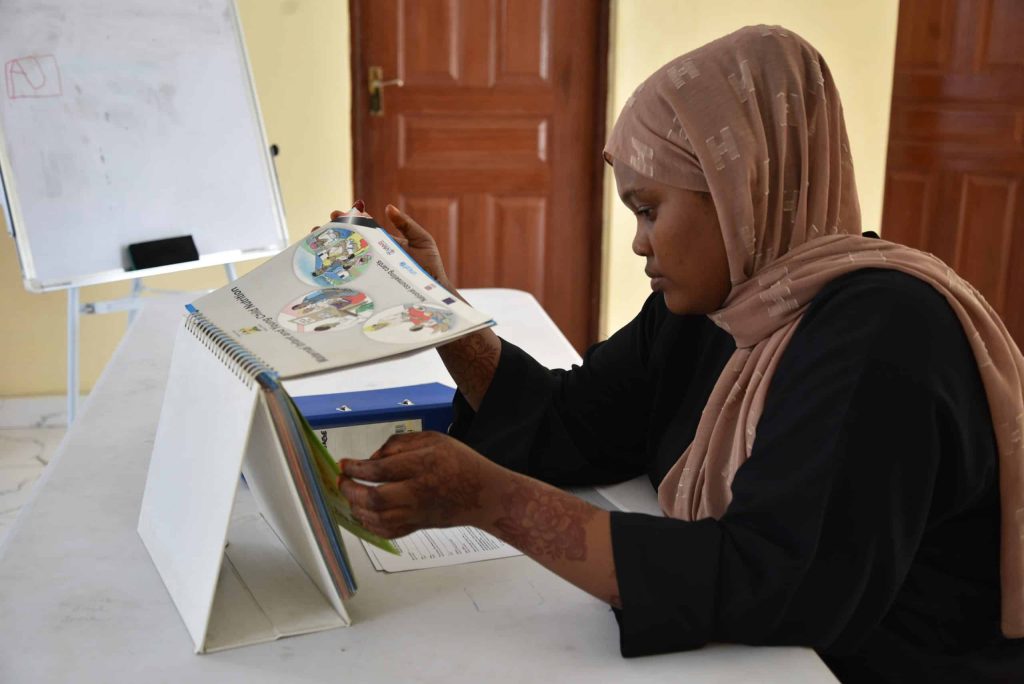
MSF also organises regular outreach activities, alongside local community-based organisations, and in conjunction with community representatives and peers, in youth-friendly spaces. Here, MSF teams provide health promotion activities, sexual and reproductive healthcare, mental health services, medical and psychosocial follow-up for survivors of sexual and gender–based violence, family planning services, and treatment for HIV and hepatitis.
The programme also includes a social component, with activities and advice on nutrition, hygiene, economic empowerment, legal access, protection and mentorship.
Two years since the project started, MSF and the Mombasa Department of Health have launched a study aimed at young people aged 10 to 24 to collect information on their health and wellbeing so as to improve available services and design better health programmes that are tailored to their needs.


Médecins Sans Frontières/Doctors Without Borders (MSF) runs a range of medical services in Kenya, including treatment of chronic and infectious diseases, healthcare for refugees and drug users, and treatment for victims of violence. Since January 2022, MSF teams in Mombasa have provided 7,087 primary healthcare consultations, 164 mental health consultations and conducted health promotion sessions with close to 8,700 people. MSF has also provided training to healthcare workers in Mombasa on caring for survivors of sexual and gender-based violence on stigma and discrimination, and has trained peer educators and others in psychological first aid.












