The morning sun rises over the green mountains of Kashmir as Taheem Jafar prepares for another day as a community mental health worker with Doctors Without Borders India/Médecins Sans Frontières (MSF). It’s 9:00 AM, and she’s already gathering her materials—information leaflets, her diary, and a pen in one of the Primary Health Centers (PHC) in Sopore, Kashmir along with her colleagues.
Morning Briefing: Planning the Day Ahead
“Our day starts at 9 AM” explains Taheem, who has been with MSF since November 2020. “At the clinic, we first check our activities for the day and discuss strategies—what material we need, which locations we’ll visit, which groups we’ll meet.”
Inside the PHC, the team assembles around a worn wooden table. Maps of surrounding villages dot the walls alongside posters explaining mental health conditions in simple terms and local language. “Today we’ll conduct visits in this area,” she says, pointing to a location on the map. “Then we have a women’s group session in the house of a community member at noon, followed by a meeting with local ASHA workers.”
The team reviews notes from previous visits, identifying families that might need follow-up. They load their bags with informational materials written in Urdu and Kashmiri, carefully designed to be accessible to those with limited literacy.
Firdaus Basheer, along with his colleagues, has to keep safety concerns in mind to plan their daily work. “We have to keep track of security concerns, which can prevent us from reaching planned locations.” His reminder is met with knowing nods—safety assessments are a routine part of their planning. The team also has to monitor the overall security situation, from security concerns to seasonal challenges like difficult terrain during winter and occasional wildlife encounters in remote areas.

Into the Community: Building Trust Through Presence
By 10 AM, the team starts with door-to-door activity in a village of modest homes with traditional wooden architecture. Children playing cricket in a small field pause as the MSF vehicle pulls up. Some recognize the team and wave enthusiastically.

The team splits up, each taking different sections of the village. Before separating, Sabreena Hassan, MSF health promotion supervisor, shares advice with newer team members: “Remember, we’re not here to diagnose or label. We’re here to listen, educate, and connect people with services if they need them.”
Rayees Ahmed Mir and Taheem Jaffar, MSF community mental health workers approaches a house where an elderly man sits on the porch. “Assalamu alaikum,” he greets. “I’m Taheem from MSF. We provide free mental health services in the area. May I talk with you for a few minutes?”

The man gestures for them to sit. “What exactly do you mean by ‘mental health’?” he asks skeptically.
This is a question Rayees and Taheem has answered countless times. “Just as our bodies can get sick, our minds can also experience difficulties, especially after stressful events. Feelings of sadness that don’t go away, trouble sleeping, constant worry—these are all signs that someone might need support.”
He explains MSF’s services carefully, emphasizing that they’re free and confidential. “Whatever is discussed remains between the person and their counselor. No one else needs to know.”
Door-to-Door: Meeting People Where They Are
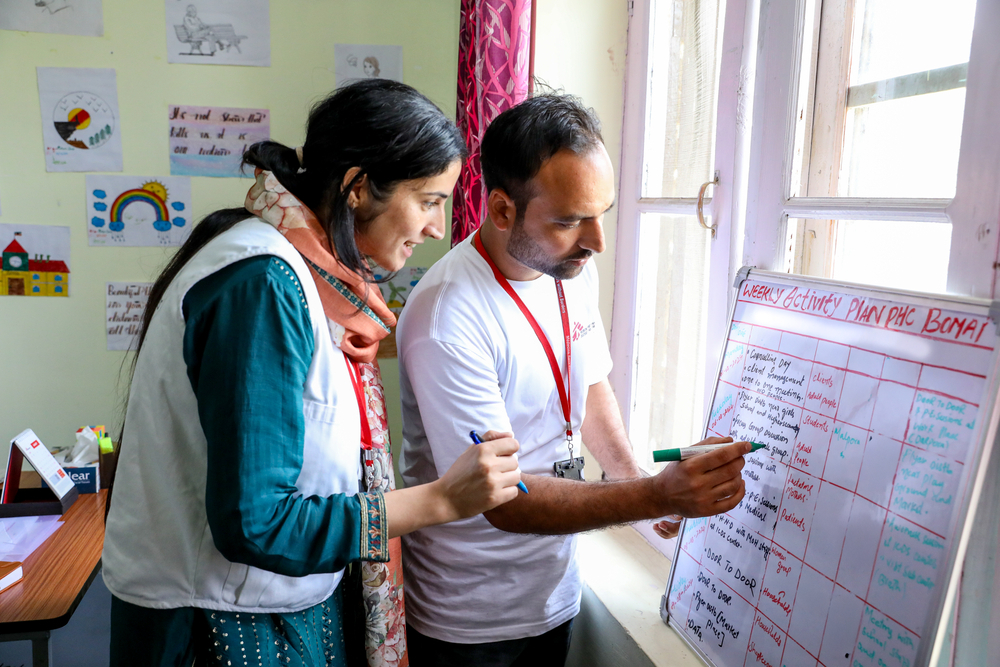
The day is quite similar for MSF Community mental health workers, the only difference is the terrain and their defined approach as per the community members. Zainab-U-Nisa and Mudasir Ahmad Lone, MSF community mental health workers, reviewing their daily schedule at Bomai Primary Health Center in Baramulla, Kashmir. Teams have to walk in a difficult terrain to reach community members and conduct outreach activity.
At a home in Bomai, Baramulla, Zainab and Mudasir Ahmad Lone are invited inside by a woman in her forties. The living room is simple but spotlessly clean, with cushions arranged on the floor around a low table.

Zainab listens attentively, noting signs of possible secondary trauma in the woman herself—the nervous hand movements, the quick glances toward the window at each passing sound.
“You’re not alone in this experience,” Zainab assures her. “Many families in Kashmir face similar challenges. Would you be interested in learning some techniques that might help both you and your husband?”
She explains how stress affects the body and mind, demonstrating a simple breathing exercise. Then she provides information about MSF’s counseling services, explaining how the woman’s husband could benefit from professional support.
“Some people think seeking help for mental health means you’re weak or crazy,” Zainab says. “But it’s actually a sign of strength—like going to a doctor when you have a physical illness.”
The woman hesitates, then asks, “Can you tell me about someone else who went for counseling? Did it help them?”
This is a common question, and Zainab is prepared. She shares the story of another family (without revealing identifying details), explaining how counseling helped them cope with similar challenges. The woman nods thoughtfully, taking the information leaflet Zainab offers.
Noon: Community Session

By midday, the team in Baramulla district converges at the house of a local community member, where fifteen women have gathered. Some have brought their young children, who play quietly in a corner with toys provided by the center staff.
Rayees Ahmed Mir and Taheem Jaffar, MSF community mental health workers starts the session by asking the women what they know about mental health. Initially, the responses are hesitant.
“It’s when someone behaves strangely,” one woman suggests.
“It’s a punishment for sins,” says another.
Taheem acknowledges each response without judgment. “These are common beliefs,” she says. “Let me share what medical science tells us about mental health.”
The session becomes more interactive as women begin sharing experiences—sleep disturbances, persistent sadness, physical symptoms like headaches and digestive problems that doctors couldn’t explain. Rayees and Taheem validate these experiences while providing information about coping strategies and available services.
“What if my husband doesn’t want me to seek help?” one woman asks quietly.

This is a challenge the team encounters frequently. Rayees steps in: “We’ve found that involving respected community figures—like religious leaders or teachers—can sometimes help family members understand the importance of mental healthcare. We can also provide family education sessions where everyone learns together.”
By the end of the two-hour session, several women express interest in follow-up consultations. The team arranges appointments at the PHC, working around the women’s household responsibilities to ensure they can attend.
Afternoon: Collaboration with Local Health Workers
After a quick lunch break, the team meets with local ASHA workers in a small community hall. These government-appointed community health workers are vital partners in reaching more people, especially in remote areas.
“Before we started working with MSF, we didn’t know how to respond when we encountered mental health issues during our home visits,” says one ASHA worker with eight years of experience. “Now we can identify warning signs and know where to refer people.”

“Remember, your relationship with families gives you a unique opportunity to reduce stigma,” Mudasir tells the ASHA workers. “When you normalize talking about mental health, it gives others permission to do the same.”
The collaboration extends beyond ASHA workers. Sabreena explains how they’ve engaged with various community stakeholders: “We conduct regular meetings with village heads, religious leaders, teachers, and even local pharmacists. In the beginning, some faith healers saw us as competition, but over time, many have become partners. Now they often refer people to us when they recognize signs of mental health conditions.”
This multi-layered approach has been crucial in creating a more supportive environment for people seeking help. As one ASHA worker notes, “Now when I suggest someone might benefit from counseling, families are much more receptive than they were three years ago.”
The Impact: Stories of Change
During a brief tea break, the team shares success stories that keep them motivated despite the challenges of their work.
Mudasir recounts the story of a woman whose husband died, leaving her alone with six children. “When we first met her, she was barely functioning. Her two oldest daughters had to drop out of school to care for the younger ones, and they were showing signs of trauma themselves. The family was isolated—relatives had helped initially but eventually returned to their own lives.”
The team provided counseling to the mother and children, initially meeting them in their home because they were reluctant to visit the clinic. “It took time and patience,” Mudasir explains. “We had to build trust gradually. The mother feared judgment from the community if people knew they were receiving mental health support.”
After several months of consistent support, changes became evident. “The mother started functioning better, and with our help, she connected with an NGO that provided financial assistance. Her daughters returned to school, and one is now preparing for medical college entrance exams.”
The most significant outcome, according to Mudasir, is that this woman now actively refers others to MSF’s services. “She’s become an advocate in her community. When she sees someone struggling, she tells them, ‘I know a place that can help.’”
Zainab shares another story about an adolescent who hadn’t left his house for six years due to severe depression. “When he first came to our clinic, he wouldn’t make eye contact or speak. After six counseling sessions, we saw remarkable changes. Now he has a job and interacts confidently with others. His parents say it’s like having their son back.”
These stories represent the tangible impact of MSF’s mental health program, which has been operating in Kashmir since 2001, providing free, high-quality, and confidential services across Kashmir valley.

Evening: Documentation and Reflection
By 4 PM, all the team returns to their respective PHCs to document their day’s activities. Each member carefully records who they met, what they observed, and any referrals made. This documentation is crucial for tracking progress and identifying patterns in the community.
“We create both qualitative and quantitative data,” explains Zainab. “This helps us understand if our strategies are working and where we need to adapt.”
The day concludes with a team reflection session. Each member shares challenges they encountered and successful moments they experienced. This practice helps them process the emotional weight of their work and learn from each other’s approaches.





For self-care, team members have developed various strategies. Zainab enjoys cooking and spending quality time with her child. Taheem practices his faith and tends to his garden. Some team members like to read books and some engage in agricultural activities on their family’s land.
“These practices help us recharge so we can return the next day with renewed energy,” says Rayeez.
Beyond the Day: The Lasting Impact
As 5 PM approaches and the team prepares to leave, their conversation turns to the broader impact of their work over the years.
This shift is evident in multiple ways: increased self-referrals to the clinic, community members openly discussing mental health issues during sessions, and even former patients becoming advocates for mental health awareness.
“One of the most significant changes,” notes Firdaus, “is that people are beginning to understand that mental health conditions are treatable. This gives hope, especially in a region where conflict and uncertainty have been constants for decades.”

The team’s work is part of MSF’s long-term commitment to supporting mental health in Kashmir. Despite challenges—constraints, deep-rooted stigma, limited resources—MSF has maintained consistent services, adapting approaches to meet evolving needs.
“Before joining MSF, I couldn’t understand people’s feelings and emotions,” reflects Taheem as the team disbands for the day. “Now my vision has changed. I see mental health as integral to overall well-being, and I’ve learned that with the right support, people have remarkable capacity for resilience and recovery.”
As the sun sets behind the mountains, casting long shadows across the valley, the team members head home—carrying with them the stories they’ve heard, the connections they’ve made, and the knowledge that their presence in these communities is slowly breaking silence and building pathways to healing.
Through their daily work—door by door, conversation by conversation, session by session—MSF’s mental health workers are changing the narrative around mental health in Kashmir, bringing professional care to those who need it most, and demonstrating that even in the most challenging contexts, healing is possible.













