They walked in single file through the narrow alleyways, winding away from their tin shack in Cape Town towards the health centre. Keitu – just 11 years old – carried her baby brother on her back since their mother was too frail and could barely manage on her own. Keitu kept a close eye on her two other little brothers as well. They had been acting out since their father died of drug-resistant tuberculosis (DR-TB) several months earlier, and they were grumpy from not having eaten anything but porridge in the last three days.
The nurse working in the health centre had begged them to come in. Keitu’s mother had been diagnosed with DR-TB as well and, since the family all breathed the same air within their one-room dwelling, there was a chance the children might have it too. The boys – aged four and six – and the baby were too young to understand, but Keitu knew enough to be afraid.
She had watched her father waste away for seven months, even though he took all his medicine before he died. His skin had turned orange; at the end, he was too weak to respond to her silly songs or whispers of “I love you” as he gasped for breath on his thin mat. Keitu chanted quietly to the children during their difficult walk, “Be brave, be brave, be brave.”

Keitu was right to be afraid. Half a million people become sick with DR-TB each year and the disease is often ruinous for families. Not only is DR-TB potentially fatal, households often incur catastrophic costs when a member of the family falls ill. Unfortunately, the current global approach to DR-TB does very little to address the disease in a family-friendly way. Although the World Health Organization (WHO) recommends that all household contacts of people living with DR-TB be assessed as quickly possible after someone in the family is diagnosed with the disease, poorly resourced programmes can do little more than make lists of the contacts who might have been exposed.
Out-dated and ineffective methods of screening for DR-TB mean that many people who are sick are simply missed. This problem is especially significant among children since many cannot produce the sputum needed to diagnose DR-TB. Instead, children have to undergo gastric washing, an intrusive and painful procedure, where a long tube is placed down a child’s nose into their stomach to try and suck out any sputum they may have swallowed, to confirm if they have TB.
Globally, very few household contacts are offered access to preventive treatments after exposure, even though this is recommended by the WHO and reduces the risk of developing DR-TB by 90 per cent. If a sick child is found, they are often taken from their family and held in a hospital for months to receive treatment, disrupting family bonds, and normal school and social activities.
In many places, children are not able to access the most effective medications, including newer drugs like bedaquiline and delamanid, because they were not included in studies of these lifesaving treatments. Instead, they are given old, often toxic, medications, which come as adult-sized tablets that have to be cut, crushed and mixed before they can be given to children.
In the worst instances, children are still treated with a daily injection, even though there are more effective oral options. These injections are not only extremely painful, but also put their hearing at risk, a devastating complication for a developing child.
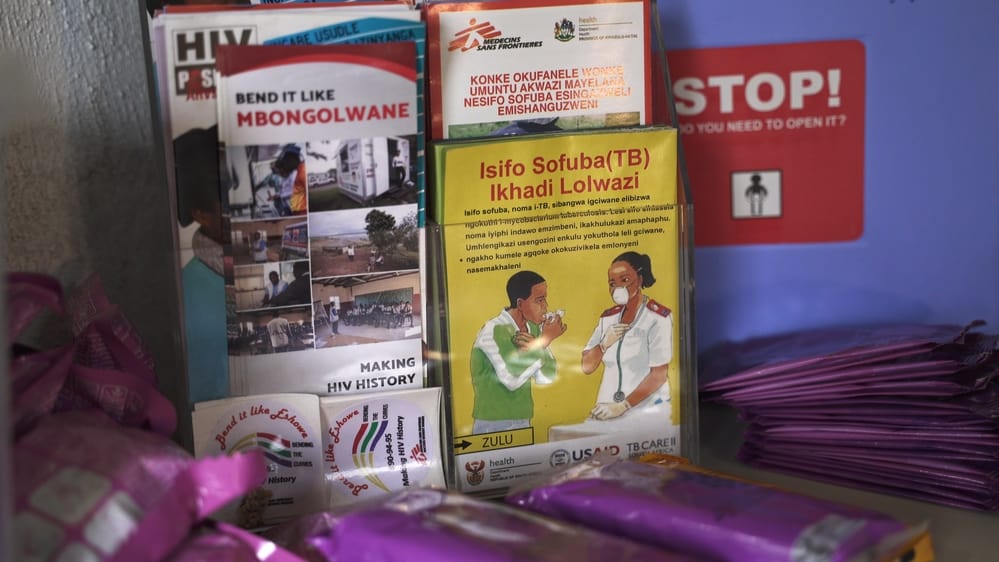
Doctors Without Borders (MSF) is addressing these family issues in our projects in South Africa and India. Through our ‘post-exposure protocols’, we are actively seeking out people who may have contracted DR-TB, and screening all children and adolescents in a household where someone has been newly diagnosed.
We are piloting the use of stool samples, rather than gastric washing, to test whether children have TB in both hospital and community settings. MSF always provides treatment free of charge and addresses the socio-economic needs of the families we serve through transportation support and food parcels, and by working with partner organisations to address other social needs.

In one project in South Africa, MSF is giving children and adolescents, who have been exposed to DR-TB, but not yet sick, preventive treatments to dramatically decrease their chances of developing DR-TB. By actively looking for the disease in exposed children, we are finding those who are infected much earlier, allowing us to treat most of them in a community setting.
In South Africa, all children receive injectable-free treatments, and in both South Africa and India, MSF has introduced child-friendly formulations of some of the most commonly used medications. We have also ensured that children in the places where we work have access to new, highly-effective TB drugs, including bedaquiline and delamanid, and that they can be treated with shorter regimens. We also provide them with nutritional support and have developed family-friendly counselling programmes to ensure their mental wellbeing is supported while they are receiving treatment.

Fortunately for Keitu, a family-centred approach was offered to them at the clinic. She, the baby, and her six-year-old brother were found to be well and were started on preventive therapy. Her four-year-old brother had been losing weight and his chest X-ray was abnormal. He was started on treatment for DR-TB after a stool sample was collected and the disease was confirmed. He was able to get an all-oral regimen with dispersible tablets, which his mother gave him each day with yoghurt. In spite of their challenges, the family began to heal and hope returned to their home.
While MSF’s work has benefitted hundreds of children and families, there are tens of thousands in need of such innovative approaches. Keitu and her family faced a challenging journey, as do thousands of families grappling with DR-TB every day. Stakeholder commitment and far greater resources are desperately needed to rapidly increase the scope of these child-friendly initiatives. This is the only way to ensure that families, like Keitu’s, face a less frightening future when one of their number becomes sick with DR-TB.
-
Related:
- India
- Paediatric TB
- South Africa
- Tuberculosis