Catastrophic events such as war and natural disasters not only affect people’s physical health, but also their mental well-being. That is why mental health services have been an important component of MSF’s emergency work for over two decades. Today, our mental health teams work in nearly 50 countries with people who have lived through difficult or traumatic experiences – ranging from victims of natural disasters to survivors of sexual violence and people living with life-threatening diseases. To mark World Mental Health Day, we bring you a snapshot of the work your support enables.

Delhi
MSF has been working in Delhi’s Jahangirpuri area since November 2015 to treat survivors of sexual and gender-based violence (SGBV).
MSF views sexual and gender-based violence (SGBV) as a medical emergency. Survivors of SGBV require immediate medical care in order to limit some of the serious consequences to their health, such as unwanted pregnancy and sexually transmitted infections. Violence can also affect the mental health of survivors, and lead to anxiety, depression and post-traumatic stress disorder.
In addition to treatment of injuries and prevention of HIV/AIDS, unwanted pregnancy, sexually transmitted diseases, our teams offer psychosocial support to reduce the risk of psychological complications which can occur as a result of violence.

Jammu and Kashmir
Years of conflict in Jammu and Kashmir have taken a toll on people’s mental health in the state. According to a survey conducted by MSF in 2015, nearly 1.8 million adults (45 per cent of the adult population) in the Kashmir Valley show symptoms of significant mental distress. This is compounded by the stigma associated with mental illness.
In response, MSF has been providing free, high-quality counselling to people affected in the valley since 2001. Currently, our teams provide counselling services at hospitals in four districts – Baramulla, Bandipora, Pulwama and Srinagar. To combat the stigma associated with mental illness, MSF teams also raise awareness on the importance of mental health and the need for the availability of mental health services in the valley.

Maharashtra
In Mumbai, MSF has been running a clinic since 2006 to treat patients with drug-resistant tuberculosis. Highly drug-resistant forms of TB are much harder to cure than drug-sensitive TB as the standard TB drugs don’t work, and the limited treatment available involves long, complex, toxic and expensive treatment. This takes a toll on patients psychologically as much as physically.
MSF believes the fight against TB requires a comprehensive, patient-centric approach. That is why in addition to new drugs, we provide psychosocial assistance to help patients cope with stigma, depression and the side effects of their medication. Our counsellors help patients remain motivated through the course of an extremely difficult treatment.
MSF also runs a programme to treat drug-resistant TB, HIV and hepatitis C in Manipur. Here too, we provide counselling to ensure a successful outcome for patients.
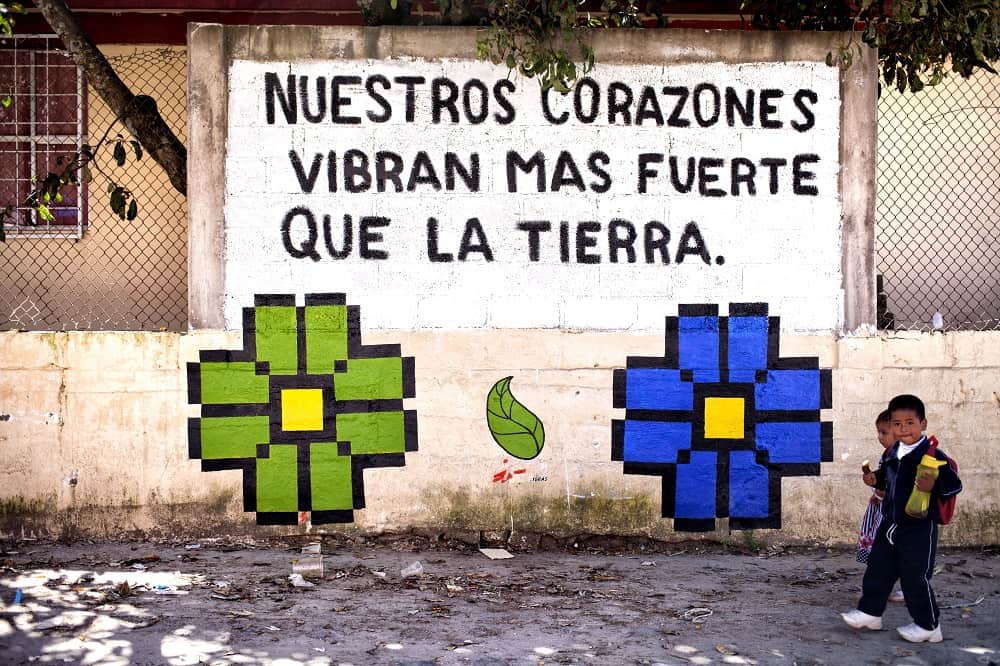
Mexico
In September 2017, several states in Mexico were affected by earthquakes which left hundreds dead, thousands injured, and many people homeless. In response, MSF deployed seven teams across Oaxaca, Puebla, Morelos, State of Mexico and Mexico City in an intervention that lasted more than two months.
Mental health services were a crucial aspect of the intervention. In Puebla, for instance, MSF teams found that survivors were affected most by the loss of all their belongings and, in many cases, by the deaths of family members and neighbours. As these are small communities, the deaths had an enormous impact on all residents, which made the individual and group mental health interventions provided by MSF all the more relevant.
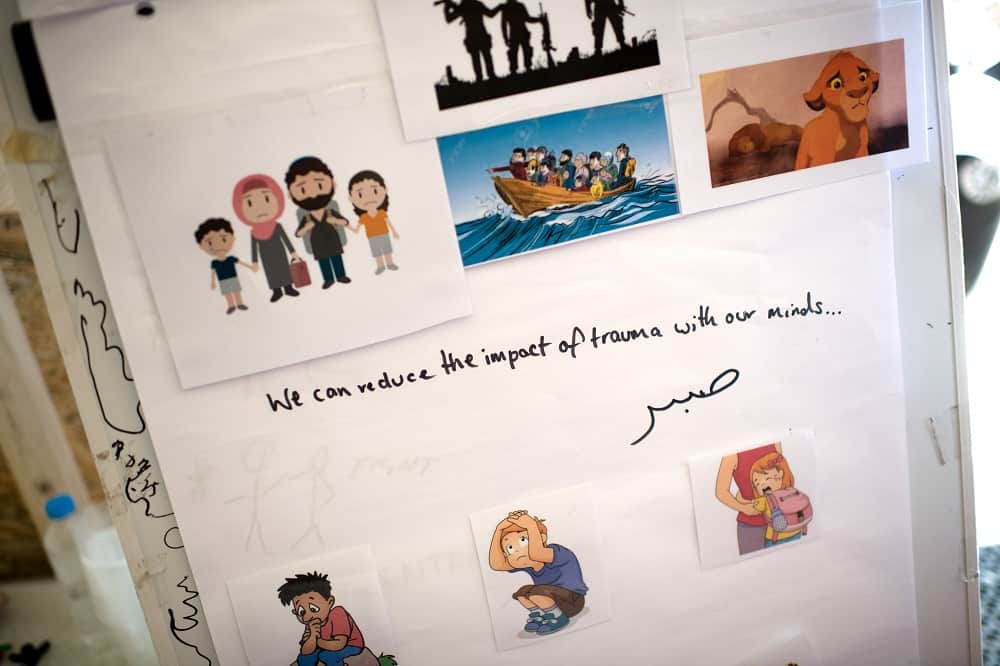
Greece
People trying to reach Europe via Turkey and the Aegean Sea have been trapped for an indefinite period of time on islands in Greece as part of the EU-Turkey deal. In Lesbos’s Moria camp, there are more than 9,000 people in a space capable of holding 3,100 people. A third of the camp’s inmates are children.
“These children come from countries in war, where they have experienced very extreme violence and trauma. Rather than receiving care and protection in Europe, they are instead subjected to ongoing fear, stress and episodes of further violence, including sexual violence,” says Dr Declan Barry, MSF’s medical coordinator in Greece.
MSF teams provide medical care and mental health support outside the camp and run a clinic for severe mental health cases in Mytilene, the capital of the island. In light of the severe mental health situation, MSF recently called for the emergency evacuation of all vulnerable people, especially children, to the Greek mainland and within the European Union.

Democratic Republic of Congo
The North Kivu region of Democratic Republic of Congo that borders Rwanda and Uganda has been in a state of constant unrest since the mid-1990s. In Mweso, a small town in the region, MSF has been providing mental healthcare to local communities and people displaced by conflict since 2009.
The team consists of psychosocial counsellors drawn from the communities surrounding Mweso. Coming from the same communities as their clients, the Mweso team understands all too well the social taboos around mental health, as well as the traumatic events people are subjected to on an almost daily basis. Conflict, armed robberies, and sexual and domestic violence are just some of the issues people face in North Kivu.
The mental health team uses theatre as a psycho-educational activity to make people aware of their problems and how to overcome them. Alongside, the team also provides therapeutic counselling for traumatic experiences such as sexual violence, psychological first-aid, psychosocial stimulation for nutrition, individual counselling and support groups for people living with conditions such as HIV, TB and diabetes, as well as referrals for psychiatric care.











